In the constantly evolving landscape of the medical and healthcare industry, the acquisition of specialized knowledge and skill sets through professional training emerges as a strategic imperative for practitioners seeking to navigate the complexities of contemporary healthcare paradigms. This discourse aims to deeply analyze the multifaceted utility of professional training in medicine and healthcare, elucidating its transformative impact on practitioner competence, industry compliance, and patient outcomes.
Technical Overview of Professional Training in Medicine and Healthcare
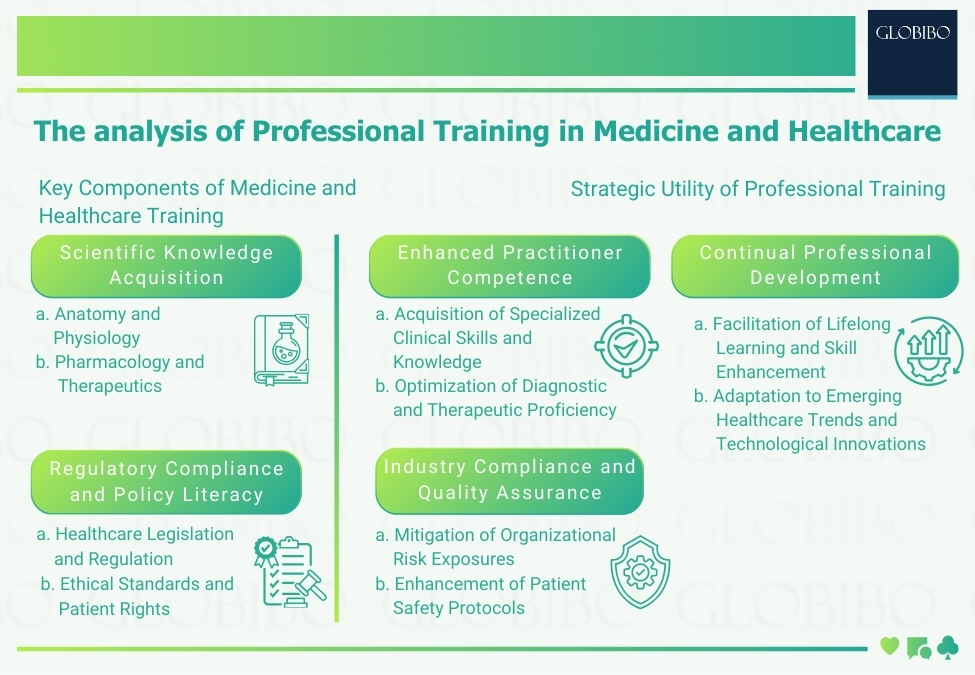
Professional training in medicine and healthcare encompasses a diverse array of specialized programs tailored to address the evolving needs of practitioners across various domains within the healthcare ecosystem. These programs focus on two key components:
1. Scientific Knowledge Acquisition
Professional training programs facilitate the acquisition of foundational scientific knowledge essential for informed decision-making and evidence-based practice within clinical settings. Practitioners undergo comprehensive instruction aimed at fostering a robust understanding of the biological underpinnings of disease pathology and therapeutic interventions. Key areas of scientific knowledge acquisition include:
- Anatomy and Physiology
- Pharmacology and Therapeutics
- Pathophysiology and Disease Mechanisms (AAMC 2021)
2. Regulatory Compliance and Policy Literacy
Given the intricate interplay between healthcare delivery and regulatory frameworks, professional training equips practitioners with the requisite expertise to navigate complex policy legislations governing clinical practice, patient privacy, and healthcare reimbursement. Through targeted coursework and case-based analyses, practitioners develop a nuanced understanding of legal obligations, ethical considerations, and compliance imperatives shaping contemporary healthcare delivery models. Key aspects of regulatory compliance and policy literacy include:
- Healthcare Legislation and Regulation
- Ethical Standards and Patient Rights
- Healthcare Reimbursement Models and Compliance Protocols (Batalden, M 2016)
Key Components of Professional Training in Medicine and Healthcare
Scientific Knowledge Acquisition
- Anatomy and Physiology: Understanding the structure and function of the human body is fundamental for healthcare practitioners to diagnose and treat medical conditions effectively.
- Pharmacology and Therapeutics: Knowledge of pharmaceutical agents and their therapeutic uses is essential for prescribing appropriate medications and managing patient care.
- Pathophysiology and Disease Mechanisms: Understanding the underlying mechanisms of diseases enables practitioners to make accurate diagnoses and develop effective treatment plans (Donaldson .2000).
Regulatory Compliance and Policy Literacy
- Healthcare Legislation and Regulation: Awareness of laws and regulations governing healthcare practice ensures that practitioners adhere to legal requirements and provide high-quality care while minimizing legal risks.
- Ethical Standards and Patient Rights: Adherence to ethical principles and respect for patient autonomy are paramount in maintaining trust and professionalism in healthcare delivery.
- Healthcare Reimbursement Models and Compliance Protocols: Understanding reimbursement systems and compliance protocols is essential for managing healthcare finances effectively and ensuring accurate billing practices (Elwyn & Thomson 2010).
Strategic Utility of Professional Training in Medicine and Healthcare
Enhanced Practitioner Competence
- Acquisition of Specialized Clinical Skills and Knowledge: Professional training equips practitioners with the skills and knowledge necessary to provide high-quality, evidence-based care across a range of medical specialties.
- Optimization of Diagnostic and Therapeutic Proficiency: Training programs focus on honing diagnostic and therapeutic skills to improve patient outcomes and reduce medical errors.
- Promotion of Evidence-Based Practice and Clinical Decision-Making: By emphasizing the importance of evidence-based practice, training programs help practitioners make informed decisions and provide the best possible care to their patients (Frenk,J .2010).
Industry Compliance and Quality Assurance
- Mitigation of Organizational Risk Exposures: Compliance with regulatory requirements and quality standards helps healthcare organizations minimize legal and financial risks associated with non-compliance.
- Enhancement of Patient Safety Protocols: Training in patient safety protocols and quality improvement strategies enables healthcare organizations to create safer environments for patients and improve clinical outcomes.
- Alignment with Regulatory Standards and Accreditation Requirements: By ensuring compliance with regulatory standards and accreditation requirements, healthcare organizations demonstrate their commitment to providing high-quality care and continuous improvement (Institute of Medicine, 2001).
Continual Professional Development
- Facilitation of Lifelong Learning and Skill Enhancement: Professional training programs promote a culture of lifelong learning, allowing healthcare practitioners to stay updated on the latest medical advancements and best practices.
- Adaptation to Emerging Healthcare Trends and Technological Innovations: Continuous professional development enables practitioners to adapt to changes in healthcare delivery, including advancements in medical technology and shifts in patient demographics.
- Promotion of Resilience and Adaptive Expertise: By fostering resilience and adaptive expertise, professional training programs help practitioners navigate challenging situations and respond effectively to unexpected events (Irby, D. & O’Brien, B. 2010).
Conclusion
In summation, the strategic imperative of professional training in medicine and healthcare transcends conventional paradigms, constituting a linchpin of practitioner competence, industry compliance, and patient-centered care delivery. Through the acquisition of specialized knowledge, regulatory literacy, and continual professional development, practitioners emerge as catalysts for transformative change within the healthcare ecosystem, driving innovation, optimizing clinical outcomes, and advancing the collective pursuit of optimal health and wellness.
Key Articles:
References
- Association of American Medical Colleges. (2021). Core Entrustable Professional Activities for Entering Residency: Curriculum Developers’ Guide.
- Batalden, M., Batalden, P., Margolis, P., Seid, M., Armstrong, G., Opipari-Arrigan, L., & Hartung, H. (2016). Coproduction of healthcare service. BMJ Quality & Safety, 25(7), 509-517.
- Donaldson, M. S., Corrigan, J. M., & Kohn, L. T. (Eds.). (2000). To err is human: building a safer health system. National Academies Press.
- Elwyn, G., Laitner, S., Coulter, A., Walker, E., Watson, P., & Thomson, R. (2010). Implementing shared decision making in the NHS. BMJ, 341, c5146.
- Frenk, J., Chen, L., Bhutta, Z. A., Cohen, J., Crisp, N., Evans, T., … & Zurayk, H. (2010). Health professionals for a new century: transforming education to strengthen health systems in an interdependent world. The Lancet, 376(9756), 1923-1958.
- Institute of Medicine (US) Committee on Quality of HealthCare in America. (2001). Crossing the quality chasm: A new health system for the 21st century. National Academies Press.
- Irby, D. M., Cooke, M., & O’Brien, B. C. (2010). Calls for reform of medical education by the Carnegie Foundation for the Advancement of Teaching: 1910 and 2010. Academic Medicine, 85.

